Endoscopic Discectomy
Minimally Invasive Spine Surgery
Herniated discs are a common spine disorder, causing thousands of patients anything from slight discomfort to intense pain and limited mobility every year. As Austin’s leading orthopedic surgeon, Dr. Dryer wants all of his patients to understand the back and neck issues they may be experiencing, as well as the procedures needed to treat them.
Up and down your spine, vertebrae are separated by tissues known as discs. These vertebral discs act as cushions that can compress, expand, and flex to allow your spine to move. They are composed of a tough outer wall and a relatively soft inner nucleus. A disc’s outer wall can become damaged through incorrect lifting of heavy objects, impact injuries, and even just normal use over time. If this happens, the nucleus may be pushed outward through the herniated wall. This can cause severe pain if the nucleus protrudes against a nearby nerve root. Because these nerves carry signals all over the body it is not uncommon for someone suffering from a herniated disc to experience pain in their arms, legs, and buttocks as well as their neck and back.
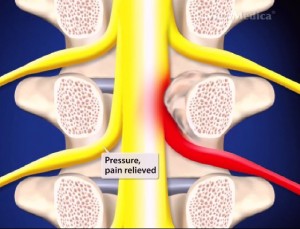
Herniated discs can be treated by a procedure known as endoscopic discectomy. This technique is only slightly intrusive, allowing access to the herniated disc through a small incision in the back. A small camera called an endoscope allows the surgeon to view the portion of the disc that is compressing the nerve root, and then remove it with surgical tools. Endoscopic discectomy is a minimally invasive surgery that usually results in shorter postoperative recovery times compared with more traditional results. However, the procedure should only be performed by an experienced orthopedic specialist such as Doctor Randall F. Dryer.
If you think you might have a herniated disc, contact the spinal experts at Central Texas Spine Institute in Austin today. To learn more about endoscopic discectomy and many other orthopedic procedures, click here.
Benefits of Endoscopic Discectomy

Reduced Tissue Trauma
There are several benefits to endoscopic discectomy compared to traditional open surgery. First and foremost, the minimally invasive nature of this lumbar spine procedure leads to reduced tissue trauma, resulting in less postoperative pain and a quicker return to normal activities. Additionally, the smaller incision size reduces the risk of infection and minimizes scarring.
Extremely Precise
Moreover, endoscopic discectomy offers a higher precision level as the surgeon can directly visualize the herniated disc and surrounding structures. This improves the accuracy of this conservative spine treatment and reduces the chances of complications, such as nerve damage. Furthermore, since the spine surgery is performed under local or general anesthesia, the patient is spared from the risks and side effects associated with general anesthesia.


Quicker Recovery
Recovery after endoscopic discectomy is generally faster compared to open spine surgery. Most patients can resume their regular activities within a few weeks, although strenuous physical activities may need to be avoided for a longer period. Physical therapy may be recommended to strengthen the back muscles and prevent future disc herniation.
Is Endoscopic Discectomy for You?
If you are experiencing symptoms of spinal disc herniation, such as back pain, leg pain, numbness, or weakness, you may be considering different spine treatment options, including endoscopic discectomy. It is important to note that not all cases of disc herniation are suitable for endoscopic discectomy. The procedure is most effective for small to moderate-sized herniations that are centrally located and not associated with significant spinal instability. A thorough evaluation by our qualified spine specialist in Austin is necessary to determine the appropriate treatment option for each individual case.
Here are some factors that can help determine if you are a suitable candidate for endoscopic discectomy:

Diagnosis:
The first step in determining if endoscopic discectomy is appropriate for you is obtaining an accurate diagnosis. This may involve a physical examination, medical history review, imaging studies (such as MRI or CT scan), and possibly other diagnostic tests. When you consult with our spine specialists, they can analyze your condition and assess the severity and location of the herniated disc.
Size and Location of the Herniation:
If the herniation is too large or located in a challenging area, open surgery or other types of spine treatment options may be more suitable. Our spine surgeon will review your imaging results to determine if endoscopic discectomy can effectively address your specific herniation.

Symptoms:
Endoscopic discectomy is typically recommended for patients who experience pain or symptoms that radiate down the legs (sciatica) due to nerve compression caused by the herniated disc. If your symptoms are primarily localized back pain without significant leg pain or neurological deficits, your healthcare provider may consider alternative treatment options, such as conservative spine therapies or medication management.

Failed Non-Surgical Spine Treatments:
In some cases, non-surgical treatments, such as physical therapy, medication, or epidural steroid injections, may not provide sufficient relief. If you have already tried and failed at conservative spine treatment options, our spine specialist may consider endoscopic discectomy as a potential solution.

Preexisting Spinal Conditions:
It is important to consider any preexisting spinal conditions you may have before opting for endoscopic discectomy. If you have spinal instability, severe degenerative disc disease, or other complex spinal issues, alternative surgical procedures may be more appropriate. Your spine surgeon will evaluate your overall spinal health to determine if endoscopic discectomy can be safely performed.

General Health and Medical History:
Your overall health and any preexisting medical conditions will influence the decision-making process for endoscopic discectomy. Certain medical conditions or medications may increase the risks associated with the procedure. It is important to provide our spine specialist with accurate information about your medical history, including any allergies, previous surgeries, or ongoing health concerns.
Ultimately, the decision to undergo endoscopic discectomy at our spine clinic in Austin should be made in consultation with a qualified spine specialist. They will conduct a comprehensive evaluation and discuss all available spine treatment options, considering your individual circumstances and goals. It is essential to have an open and honest conversation with our spine specialist to ensure that you make an informed decision about your treatment plan.
CONTACT OUR SPINE SPECIALISTS TODAY
Endoscopic discectomy is a minimally invasive treatment option for spinal disc herniation. It offers numerous advantages over traditional open surgery, including reduced tissue trauma, faster recovery, improved precision, and decreased risk of complications. However, it is essential to consult with a knowledgeable spine specialist at Central Texas Spine Institute in Austin to determine if endoscopic discectomy is the right choice for your specific condition. Call today.




